As we get older, we might expect to go to the doctor more often or need other medical help to keep us well.
It’s a natural part of the ageing process, but that’s not to say there aren’t ways to soften and slow the impact of getting older and help people to age well.
A growing, ageing population.
In the early 1970s, the population of the UK was 55.8 million, with an average life expectancy of around 71 years.
Just 50 years later, the population is over 12 million higher – 68.5 million – and we can expect to live a full ten years longer.
Population growth means an increased demand for the NHS. However, with people living for longer, a growing number of people will require more and more support to stay healthy as they get old.
The NHS’s Long Term Plan aims to help people stay in as good health as possible in those latter years through integrated and proactive health care services.
Long-Term Conditions and Frailty
A ‘long-term condition’ is a chronic disease or illness for which there is no cure and needs to be managed through medication or other treatment.
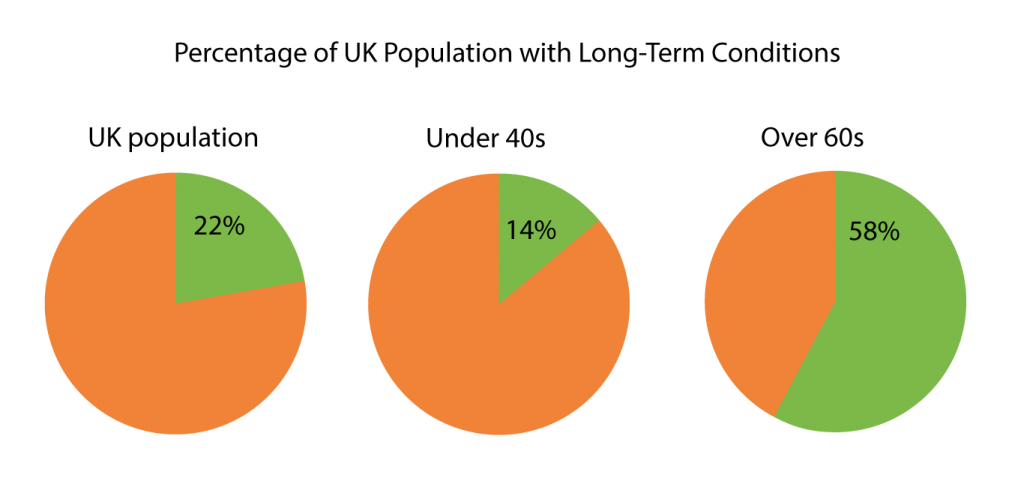
Around 15 million people in the UK have a long-term condition, and age is one of the most significant factors. In people aged 40 and under, 14% have a long-term illness, whereas, for those aged 60 or older, that figure jumps to 58%.
Dementia, hypertension (high blood pressure) and osteoarthritis are among the most prevalent conditions that impact older people’s quality of life.
While not considered a condition itself, frailty adds to the decline people can experience in old age. Frailty is a syndrome that diminishes people’s resilience along with the ageing process and long-term conditions.
Frailty creates a cycle where people are more likely to get ill, take longer to recover and become more susceptible to falls or infections.
Effectively managing long-term conditions and identifying and helping people at risk of frailty means that rapid decline in old age is not inevitable.
How General Practice helps
As well as treating people when they need it, the NHS invest heavily in preventative measures that stop people from becoming seriously ill. It increases people’s quality of life and reduces the need for larger-scale NHS intervention in the future.
For generally healthy people, there is the NHS screening programme which aims to discover the risk signs of cancer and other diseases early when they are most treatable.
The NHS will send everyone over 60 an at-home kit to screen for bowel cancer every two years, with cervical screening continuing until age 64 and mammograms (breast cancer screening) running from age 50 to 74.
Men aged 65 will also be screened for abdominal aortic aneurysms – swelling of a blood vessel that runs from the heart through the chest and tummy.
When the NHS invites you to a screening, it’s essential to make an appointment without delay.
Managing conditions and medication
For people with long-term conditions or who regularly take medications, it is vital to have a review with a health care professional at least every year.
Reviews are valuable opportunities for you to discuss your health – progress, problems and aims – with a member of the practice or Primary Care Network (PCN) team.
Practice Nurse teams will often conduct reviews, as will PCN staff like Clinical Pharmacists. Their expertise especially comes into play if people regularly take more than one type of medication.
Part of PCNs’ focus, working in partnership with GP practices, is holistically looking at people’s health. Not just one prescription or condition at a time, but to take an overall look, acknowledging that one aspect of health, wellbeing, medication or treatment can impact others.
Managing wellbeing
The more information you can give – either through a digital consultation or speaking with our trained Reception team – will help us get you the support you need as soon as possible.
Where there are non-medical factors that impact a person’s health, PCN staff like Social Prescribing Link Workers (SPLWs) play a vital role.
Factors like loneliness, isolation, stress, or financial worries are all proven to impact people’s physical and mental health negatively, and SPLWs are specialists in tackling the problems that the NHS can’t solve with medication.
For example, supporting and empowering people with limited mobility to attend a Physio-led exercise class can improve their range of movement and social interactions. You can read more about social prescribing for frailty in a previous case study.
The more information you can give – either through a digital consultation or speaking with our trained Reception team – will help us get you the support you need as soon as possible.
